Overview of lung-on-a-chip systems – The use of the alveolar-capillary barrier in human medicine
Introduction to lung-on-a-chip microfluidic systems
Organ-on-a-chip technology provides unique opportunities to study lung physiology and pathophysiology in vitro. The first lung-on-a-chip platforms emerged almost ten years ago, and significant progress has since been made in biological and engineering complexity.
Here, we describe one of the most sophisticated lung-on-a-chip systems in terms of biological complexity [1] that model the alveolar-capillary barrier to present current knowledge on the topic.
Structure and function of the human lung
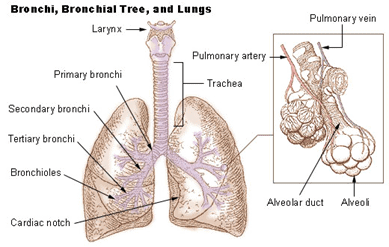
The foremost function of the lung is to supply the body with oxygen and to get rid of the waste product of respiration – carbon dioxide.
The lung has a highly branching structure. As we breathe in air, the air is driven by pressure to flow down the trachea, continuing downstream through the smaller branches until it reaches the minor structures of the lung – the alveoli.
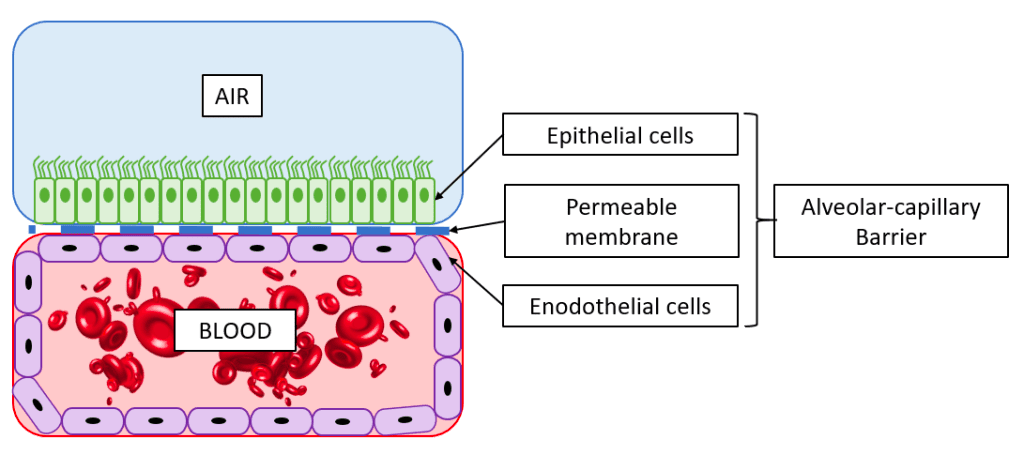
The alveoli are tiny hollow air-filled sacs surrounded by a network of capillaries. Here, in the 480 million alveoli of a human lung, the exchange of oxygen and carbon dioxide occurs. To enter the bloodstream, air molecules must cross the alveolar-capillary barrier, and likewise, the carbon dioxide must pass the barrier to exit the body during the exhale.
In-vitro models of the alveolar-capillary barrier
The alveolar barrier thus plays a vital role in allowing oxygen to enter the body, and failure of the alveoli can be a severe condition. Infection diseases in the alveoli, such as pulmonary edema or pneumonia, affect hundreds of millions of people globally and result in millions of deaths every year. Additionally, oral inhalation of drugs is a standard means of drug delivery, and understanding what substances can pass across the alveolar barrier is, therefore, of great importance.
As in most fields of biomedical research, animal models are commonly used to study lung pathology and to develop new treatments. Ethical issues limit the use of animal models for study, and animal lungs are substantially different from human lungs [2], limiting the translation of results. This has motivated the development of in vitro platforms for lung research. Read more about in vitro platforms for lung research here.
Organ-on-a-chip technology to model the alveolar-capillary barrier
The term “organ-on-a-chip,” as well as the technology, was developed by Donald Ingber, founder of the Wyss Institute at Harvard University. Organ-on-a-chip systems are essentially micro-engineered devices containing living cells that mimic the functions of human organs.
Donald Ingber’s team developed the seminal breathing lung-on-a-chip model that incorporated the mechanical cues of breathing in organ-on-a-chip devices. Following the first publication of this model, the team has published several studies to model different pathological conditions of respiratory diseases on-chip [3-6].
Lung-on-a-chip architecture
Read about the engineering aspects of lung-on-a-chip devices here.
Compared to the previous generation of lung-on-a-chip models, the most recent models developed by the Ingber group include the following novel features:
The use of human primary cells
Primary human lung alveolar epithelial cells and human vascular endothelial cells were seeded in the mode instead of the cancer cell line. This is important as primary cells can link the results to the donor they were acquired from – an essential step towards personalized medicine.
Furthermore, primary cells more truly replicate the diversity of human tissue compared to cell lines, which have developed homogeneous phenotypes due to passaging.
Microfluidic perfusion of whole blood
All four walls of the endothelial compartment of the chip were lined with a continuous layer of endothelial cells, forming a “vascular tube.” This enabled the perfusion of whole blood through the lumen of the vascular tube without thrombus formation, as it usually occurs if blood is perfused through a microchannel, even when coated with extracellular matrix proteins.
Discover how to do cell perfusion in a microfluidic chip for dynamic cell culture.
Disease modeling in microfluidic lung-on-a-chip systems
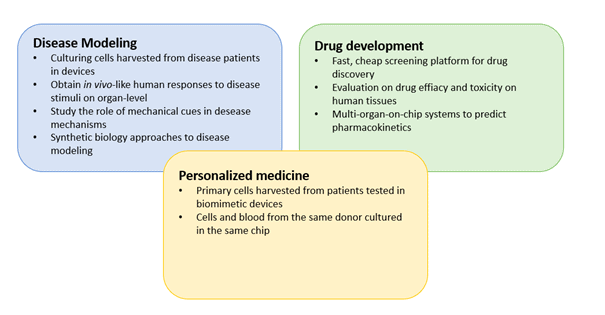
Mimicking pathological conditions in organ-on-a-chip models that accurately represent human physiology is of great interest for future drug development and fundamental research into respiratory diseases.
This culture model enabled experimental investigation of intravascular thrombosis under hemodynamic conditions. The disease state was induced by perfusing tumor necrosis factor-α (TNF-α), an inflammatory stimulant, in the fluid compartment. This resulted in disease features such as platelet aggregation dose-dependent and inflammation, as also accrues in patients exposed to TNF-α.
Furthermore, this system highlighted one of the main advantages of organ-on-a-chip systems for disease modeling: the ability to study the contribution of individual tissue components of the organ compared to their cooperative responses at the organ level. This synthetic biology approach is naturally not seen in animal studies, where only system-level responses can be obtained.
Future directions of lung-on-a-chip development
Although it proved a promising technique for future lung in-vitro research, further research is needed to develop more physiologically relevant and practical systems. The biological components of lung-on-a-chip devices are still oversimplified and lack cellular components such as immune cells or neural cells.
The study presented in this review demonstrated significant improvements by using primary cells and perfusing whole blood in the system. Furthermore, the engineering aspects, such as device material, sensor integration, and compatibility with other laboratory equipment, are expected to progress in the coming years.

Review done thanks to the support of the MaMi H2020-MSCA-ITN-2017-Action “Innovative Training Networks”
Grant agreement number: 766007
Written by
Emma Thomée, PhD
Contact:

References
- Jain, A., Barrile, R., van der Meer, A., Mammoto, A., Mammoto, T., De Ceunynck, K., Aisiku, O., Otieno, M., Louden, C., Hamilton, G., Flaumenhaft, R., Ingber, D., 2018. Primary Human Lung Alveolus-on-a-chip Model of Intravascular Thrombosis for Assessment of Therapeutics. Clin. Pharmacol. Ther. 103, 332–340. Primary human lung alveolus‐on‐a‐chip model of intravascular thrombosis for assessment of therapeutics
- Miller, A.J., Spence, J.R., 2017. In Vitro Models to Study Human Lung Development, Disease and Homeostasis. Physiology 32, 246–260.
- Benam, Kambez H., Novak, R., Nawroth, J., Hirano-Kobayashi, M., Ferrante, T.C., Choe, Y., Prantil-Baun, R., Weaver, J.C., Bahinski, A., Parker, K.K., Ingber, D.E., 2016. Matched-Comparative Modeling of Normal and Diseased Human Airway Responses Using a Microengineered Breathing Lung Chip. Cell Syst. 3, 456-466.e4.
- Benam, Kambez H, Villenave, R., Lucchesi, C., Varone, A., Hubeau, C., Lee, H.-H., Alves, S.E., Salmon, M., Ferrante, T.C., Weaver, J.C., Bahinski, A., Hamilton, G.A., Ingber, D.E., 2016. Small airway-on-a-chip enables analysis of human lung inflammation and drug responses in vitro. Nat. Methods 13, 151–157.
- Hassell, B.A., Goyal, G., Lee, E., Sontheimer-Phelps, A., Levy, O., Chen, C.S., Ingber, D.E., 2017. Human organ chip models recapitulate orthotopic lung cancer growth, therapeutic responses, and tumor dormancy in vitro. Cell Rep. 21, 508–516.
- Huh, D., Leslie, D.C., Matthews, B.D., Fraser, J.P., Jurek, S., Hamilton, G.A., Thorneloe, K.S., McAlexander, M.A., Ingber, D.E., 2012.
A human disease model of drug toxicity-induced pulmonary edema in a lung-on-a-chip microdevice. Sci. Transl. Med. 4.